The Role of Gut Microbiome in Autoimmune Diseases
In recent years, the gut microbiome has emerged as a critical player in the development and management of autoimmune diseases. The intricate balance of microorganisms residing in our intestines can significantly influence our immune system and overall health. This article explores the relationship between gut microbiota and autoimmune conditions, highlighting recent research findings that shed light on this complex interplay.
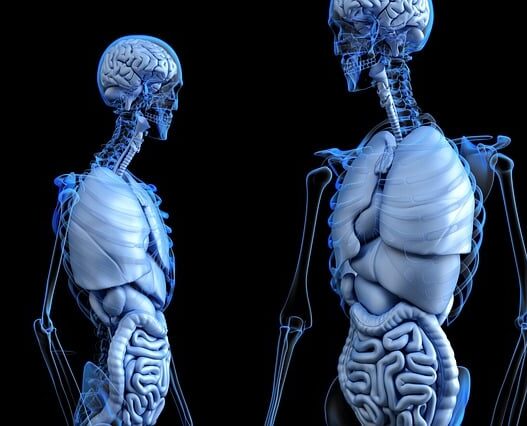
Understanding the Gut Microbiome
The gut microbiome consists of trillions of microorganisms, including bacteria, viruses, fungi, and other microbes, that reside in the gastrointestinal tract. These microorganisms perform various essential functions, such as aiding digestion, synthesizing vitamins, and regulating immune responses. However, when the balance of these microbes is disrupted—a condition known as dysbiosis—it can lead to inflammation and contribute to the development of autoimmune diseases.
Key Research Findings
The Dynamic Interplay between the Gut Microbiota and Autoimmune Diseases
Summary:
The article provides an in-depth examination of the intricate relationship between gut microbiota and autoimmune diseases. It discusses how gut microbiota can influence immune system behavior, potentially leading to the development of autoimmune conditions.
The gut microbiota influences the immune system by producing metabolites, such as short-chain fatty acids, that can modulate immune responses. These metabolites can promote anti-inflammatory pathways, which are crucial for maintaining tolerance and preventing autoimmunity.
The article emphasizes that diet significantly impacts gut microbiota composition. Specific dietary changes, including increased fiber intake and probiotic consumption, can enhance microbial diversity and promote a healthy immune response.
The Microbiome in Autoimmune Diseases
This article explores the role of the gut microbiome in autoimmune diseases, highlighting how dysbiosis—an imbalance in microbial communities—can influence immune responses and contribute to conditions like systemic lupus erythematosus, rheumatoid arthritis, and multiple sclerosis. The authors discuss mechanisms such as immune modulation and intestinal barrier integrity, emphasizing the potential of microbiome-targeted therapies like probiotics and dietary interventions to restore balance and improve autoimmune disease management.
The Impact of the Gut Microbiome on Extra-Intestinal Autoimmune Diseases
Influence of Gut Microbiota on Autoimmunity: A Narrative Review
CONCLUSION:
“Gut microbiota as explained helps in attaining immune homeostasis in the body. Its further functions are yet another scope for study in this field. The dysbiosis or its alteration caused various factors starting from genetics to environment including lifestyle causes various autoimmune conditions. Changes in the gut microbiota affect both innate and adaptive immunity by influencing the neutrophil-activating capacity, impairing CD4 and CD8 T cells, and affecting B cells, among other immune responses. This presented mechanistic evidence for future beneficial strategies based on the gut microbiota for avoiding autoimmune illnesses, which links dysbiosis of the gut microbiota with autoimmune pathways implicated in disease development.”
Emerging Role of Gut Microbiota in Autoimmune Diseases
CONCLUSION
“The interaction between human microbiota and the host plays a crucial role in maintaining health and influencing disease onset. The complex relationship encompasses multiple facets, with microbiota and their metabolites wielding significant influence over host inflammation and immune responses. The gut microbiota participates in regulating immune cell proliferation, differentiation, activation, intestinal permeability, and the integrity of mucosal barriers. Probiotics have emerged as a promising strategy for managing autoimmune diseases, such as SLE and RA. They operate by promoting a healthy gut microbiota and fostering a balanced interaction with the host’s immune system. However, further investigations are warranted to identify specific biomarkers that can accurately distinguish between healthy and compromised microbiota states. Additionally, understanding how microbiota and their metabolites impact normal balanced states versus inflammatory conditions, and discerning potential differences between effects on mucosal surfaces and systemic tissues, remains crucial. In-depth studies investigating the role of microbiota in autoimmune diseases provide insights into the underlying mechanisms of diseases. These insights may reveal prominent diagnostic markers and therapeutic targets, ultimately help us to understand the pathogenesis of autoimmune diseases and explore novel diagnostic and therapeutic strategies.”